Joint replacement
Our program
The joint replacement program at the Center for Orthopedic Excellence at Syosset Hospital is a comprehensive diagnostic and surgical treatment program for people with arthritis, degenerative and congenital problems or trauma associated with the hip and knee. Our team is committed to providing patients with the highest quality, scientifically advanced joint replacement surgery and rehabilitation to return them to their maximum level of function and mobility.
Why choose us?
The Center for Orthopedic Excellence and its dedicated team of healthcare professionals focus on you as an individual. We believe that continuity of care offers the best results, so our doctors work with you during every part of your experience and follow you through preoperative education and presurgical testing, the surgical experience itself, rehabilitation and your return to a healthy and active life. This continuity of care means that not only will you have a better experience and recovery, you'll also have an added level of comfort and reassurance that comes with seeing familiar faces throughout your care.
Our team is composed of surgeons, physicians, nurses, physician assistants, rehabilitation specialists and healthcare professionals who have been chosen specifically for their training, skill and compassion.
International leadership & recognition
More than 500 surgeons from all over the world have observed our center's experts perform joint replacements and have returned to their native countries with new surgical skills. Conversely, the team has traveled extensively overseas to provide guest lectures as well as clinical and education programs.
The team also brings its expertise abroad through philanthropic programs, regularly performing hip and knee replacements in Ghana and other areas of the world with medically underserved populations.

We have been recognized by the Joint Commission for Disease Specific Certification in spine surgery and Advanced Certification for hip and knee surgery.
If you're scheduled to undergo a total joint replacement, be sure to download our patient education brochures. You'll learn all you need to know before, during and after your total joint replacement procedure.
In Connections, Northwell experts discuss high-tech surgeries, more durable implants and new ways to control joint pain.
Wondering if your hip or knee pain warrants a visit? Our free health risk assessment may help.
About total joint replacement
When someone suffers from arthritis related to degenerative, congenital, inflammatory, or traumatic causes, it may be hard for them to perform even simple tasks such as walking or climbing stairs. They may even feel pain when sitting or lying down. A painful joint can often prevent patients from enjoying daily activities such as walking, shopping, traveling and recreational sports, leading to a sedentary life. If medications, changing everyday activities and the use of walking aids are not helpful, joint replacement surgery may be an option.
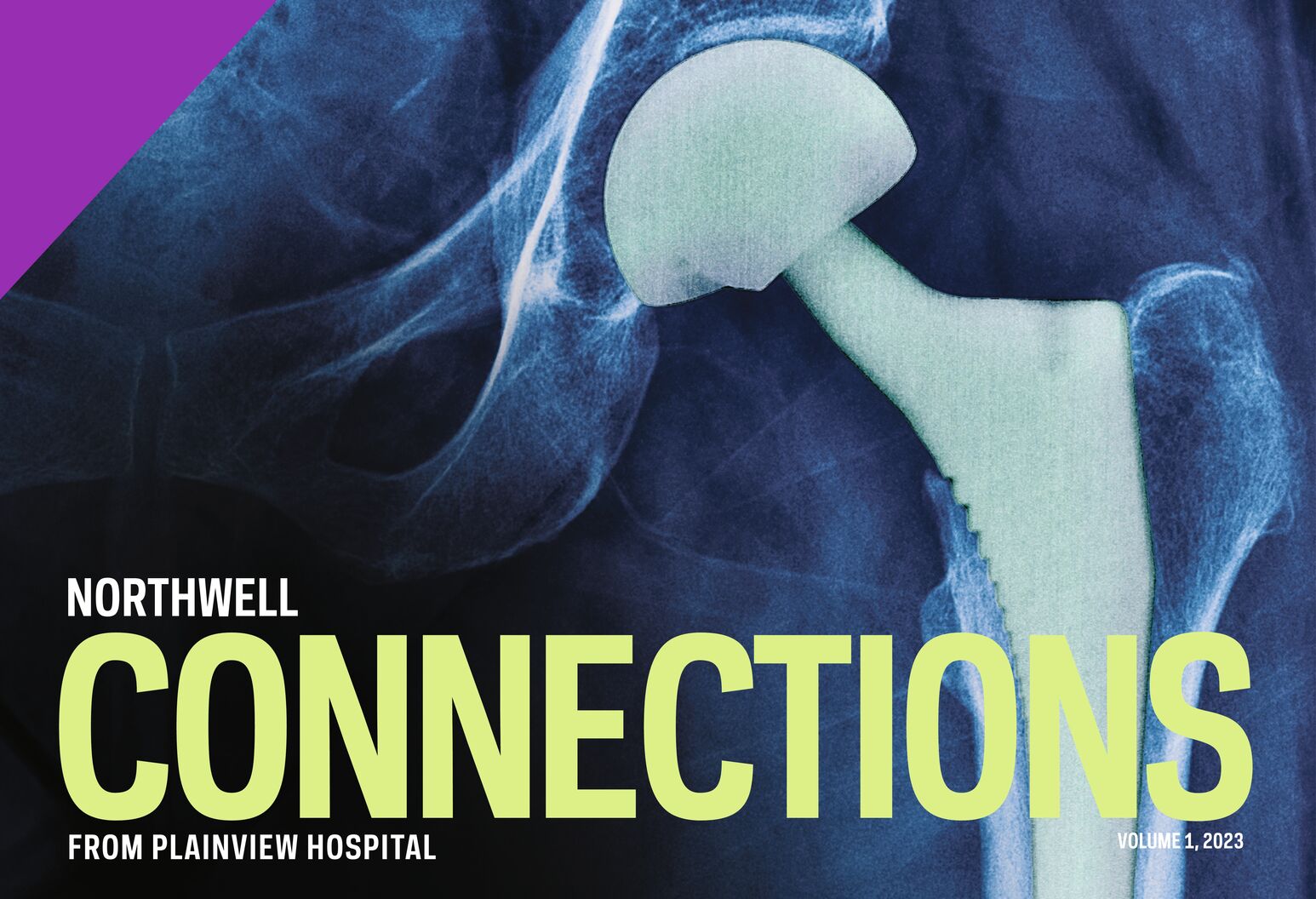
Joint replacement implants are metal and plastic coverings for raw, arthritic bone ends. They replace cartilage that has worn away over the years. Total joint replacement surgery can help relieve pain and get patients back to enjoying normal everyday activities. Replacement implants are made from materials such as titanium or other metal alloys, ceramics, plastics or other newer substances. The goal is to eliminate bone-on-bone friction to create a new, smoothly functioning joint that will last for years.
In a total hip replacement, the surgeon removes the arthritic ball of the thighbone (femur) and the damaged, inflamed cartilage in the hip socket. The ball is replaced by a metal or ceramic ball attached to a stem, placed into the thighbone. A metal cup relines the socket, creating a new, smooth and durable joint.
In a total knee replacement, the arthritic rough surfaces at the end of the thighbone and shinbone are replaced with polished metal inlays. A space-age plastic cushion separates the inlays, acting as an artificial cartilage. The kneecap (patella) is preserved and, if worn, is resurfaced with a similar plastic cushion.
Before surgery
The first visit
During your first visit, one of our surgeons will perform a thorough examination and may ask for further imaging and laboratory tests to provide the best diagnostic information for your treatment plan. This is key to a successful outcome. While at the office, you may also meet with the surgical coordinator, who can help with scheduling and logistics, as well as the patient educator and the physician assistant.
Presurgical testing
You'll have to contact the department directly to schedule a presurgical testing appointment approximately 21 days prior to surgery. Presurgical testing includes a physical examination and further laboratory tests if needed. If you are not feeling well for any reason, this should be brought to the attention of the staff. The hospital also requires a medical clearance from your primary care physician and/or specialist, such as a cardiologist. These should be obtained prior to the date of presurgical testing.
Preparation
When preparing for joint replacement surgery, as with any surgery, there are some preoperative considerations to keep in mind that can help optimize your results and recovery:
- Exercise—Our bodies tend to heal and regain function faster when they are in good physical and cardiovascular condition.
- Medication—Before the surgery, discuss medications you may currently be taking with your physician. Some may need to be temporarily discontinued until after the surgery. This determination can be most appropriately made by your physician or orthopedist.
- Discharge planning—As with any surgery, you should be sure to discuss discharge planning with your physician beforehand. The discharge plan may include instructions on care of the incision, pain medications, activities, special exercises, and other home care instructions.
- Rehabilitation—People who have received a total joint replacement can still lead functional, active lifestyles. One major component of many rehabilitation programs is exercise—to restore function, mobility, and strength to the affected joint and surrounding muscles. Discuss with your physician what an appropriate postoperative rehabilitation program should include.
Surgical options
After all the clinical data is reviewed, your doctor will decide on the optimal surgical procedure for the joint replacement. Different patients require different surgical options, so your treatment plan is tailored to your specific needs and will be presented in great detail so you understand what is involved.
Surgical options include:
- Minimally invasive techniques—The center's surgeons are skilled in using smaller incisions to perform repairs to the knee and hip.
- Revision surgery—Prosthetic joints used in joint replacement surgery have a finite life span. When that time comes, revision surgery replaces previous worn out joint replacements. These revision surgeries are even more complex than the original surgery and demand the highest level of surgical skills that orthopedic surgeons, such as those at our center, can provide.
- Anterior approach to hip replacement surgery—The anterior approach means that the surgeon reaches the hip by going between two muscles, rather than by removing and then reattaching a muscle. This can allow for less postoperative pain and faster rehabilitation and recovery.
- Robotic total joint replacement—A minimally invasive procedure performed through a small incision using a robot-guided system.
The surgical experience
The hospital will call you the day prior to surgery to remind you of the time to arrive at the hospital for the procedure. On the day of surgery, after checking in to the hospital, your records and all consent forms will be reviewed by the nursing staff and you will be brought to the presurgical holding area.
The surgeon will personally mark the specific site of surgery and the anesthesiologist will again review the options for anesthesia. The majority of joint replacement surgery is performed under regional anesthesia, however, in some instances general anesthesia is preferred. The final decision is made by you and the anesthesiologist. For those patients undergoing regional or epidural anesthesia, additional sedation can be given during the surgery.
For routine joint replacements, the actual surgical procedure generally takes less than one hour. Immediately after the surgery, you will be taken to the Post Anesthesia Care Unit (PACU) where you will be monitored for several hours before being brought to the hospital room. Your family will be notified once surgery is complete and you have been transferred to the PACU.
Rehabilitation
Rehabilitation following joint replacement surgery starts in the hospital within just a few hours of the procedure. Physical therapists and rehabilitation specialists will prescribe exercises to help you get out of bed and regain strength as safely and rapidly as possible. Most patients spend one day on the orthopedic surgical floor and are able to walk with a cane or walker and use the stairs independently when leaving the hospital.
The Northwell Health Rehabilitation Network offers results-oriented, comprehensive rehabilitation. The team members serve as your partners in care, dedicated to a safe, healthy and rapid recovery. The options include:
- Acute inpatient rehabilitation—This is designed for people who need close daily physician monitoring, 24-hour registered nurses and intensive physical, occupational and/or speech therapy to maximize recovery. We provide comprehensive programs for therapy, and other treatments for neurological disorders, cardiac conditions and orthopedic and spinal cord injuries.
- At-home rehabilitation—Northwell Health At Home provides comprehensive, specialized joint replacement home care services with an emphasis on rehabilitation, wellness and recovery in the home setting. Physical therapy will begin within 24 hours of discharge, ensuring a seamless transition from the inpatient facility to the home. Therapy intensity and duration of services will vary depending on the patient's needs, abilities, and insurance coverage. A rehabilitation nurse coordinator will serve as a liaison between the patient's physician and all home care disciplines, enhancing communication and coordination of care.
- Outpatient rehabilitation—There are many outpatient facilities across Long Island, Queens, Manhattan, Staten Island and Westchester.
- Sub-acute inpatient rehabilitation—This is short-term inpatient rehabilitation for recovery from an accident, injury or illness. It also includes skilled nursing (nursing home) services.
Our team
Ayal Segal, MD
Associate Director of Orthopaedic Surgery, North Shore University Hospital Syosset
Joshua Neil Steinvurzel, MD
Chief - Orthopaedic Surgery of Surgery - Orthopedic Surgery, Glen Cove Hospital
Baruch Toledano, MD
Co-Chief - Trauma of Orthopaedic Surgery, North Shore University Hospital
William B. Walsh, MD
Chief of Division - Chief of Orthopaedics of Surgery - Orthopaedics, Plainview Hospital